Drug companies never talk about the benefits and harms of their drugs but about their efficacy and safety. Words create what they describe and the preferred semantics is seductive. It makes you think it can only be good for you to take drugs, as they are both efficacious and safe. Another reason why patients and doctors generally trust their drugs as being both efficacious and safe is that they think they have been carefully tested by the drug industry and carefully scrutinised by the drug regulatory agencies using high standards before they are allowed onto the market.
It’s the other way round. In contrast to food and water, which are not only pretty harmless but something we need to survive, drugs are generally neither efficacious nor safe. Paracelsus stated 500 years ago that all drugs are poisons and that the right dose differentiates a poison from a remedy. Drugs always cause harm. If they didn’t, they would be inert and therefore unable to give any benefit. For all drugs, it is therefore essential to find a dose that causes more good than harm in most patients. Even when we succeed with this, most patients will still not achieve any benefit from the drugs they take.
Although it is rather obvious that drugs can kill you, this is often forgotten, both by patients and doctors. People trust their medicines to such a degree that the Canadian physician Sir William Osler (1849-1919) wrote that ‘the desire to take medicine is perhaps the greatest feature which distinguishes man from animals. A particularly amusing example is botulinum toxin, which is a neurotoxin produced by the bacterium Clostridium botulinum. It is one of the strongest poisons in nature, and a dose of only 50 ng killed half of the monkeys in a toxicity study (which means that 1 g can kill 10 million monkeys). I wonder who needed this information so badly that it was worth killing our animal relatives to get it. And yet, what is this amazing killer drug used for? For treating wrinkles between the eyebrows! This comes with age, but you shouldn’t be too old and have too much tremor when you inject the toxin, as it can be absorbed from the mucous membranes in the eye and kill you. The package insert warns that deaths have occurred. Is it really worth running a risk of dying, however small it might be, just because you have wrinkles? Other questions that pop up are: Can the drug be used for suicide or murder? Why was it ever approved?
The fact that drugs are dangerous and should be used with caution means that the ethical standards for those who do research on drugs and market them should be very high. I have talked to many people in the drug industry to find out what the companies think of themselves, and the replies have ranged from very positive ones from people who were proud of the clinical trials they carried out to very negative ones. What is perhaps more interesting is to see which impression the drug companies want to give of themselves to the public and to compare this with what they actually do. The Pharmaceutical Research and Manufacturers of America (PhRMA) claims its members are ‘committed to following the highest ethical standards as well as all legal requirements’. Its Code on Interactions with Healthcare Professionals states that:
Ethical relationships with healthcare professionals are critical to our mission of helping patients … An important part of achieving this mission is ensuring that healthcare professionals have the latest, most accurate information available regarding prescription medicines.
Here is another quotation. Under the heading, FOCUS ENGAGEMENT HONESTY, came this text: ‘Our goal is to be the world’s most successful, respected and socially responsible consumer ware producer.
As you’ll see shortly, the drug industry’s actions have very little to do with honesty, respect and social responsibility. How could they then write this about themselves? Well, they didn’t. They could have, but the quotation comes from a newspaper advertisement for Philip Morris that shows a portrait of a smiling young woman who won’t continue to look so good if she smokes.
I tell you this to illustrate that not even the most deadly industry on the planet can resist the temptation of spreading bullshit while they increase the total consumption of tobacco because their marketing is directly targeted towards teenagers in the developing countries who have not yet started smoking. This marketing more than compensates for the decline in smoking in developed countries. How can it be socially responsible to deliberately kill millions of people every year who didn’t need the product in the first place? People who have tried to smoke a cigarette know what I’m talking about. Aged 15, I only succeeded in smoking half a cigarette before I became so intoxicated that I vomited and left school to go directly to bed, as white as my sheets. My mother wondered what terrible disease had hit me so hard and told me later that she’d found half a cigarette in my shirt pocket.
The disconnect between the drug industry’s proclamations of ‘highest ethical standards’, ‘following … all legal requirements’ and ‘most accurate information available regarding prescription medicines’ and the reality of big pharma’s conduct is also vast. The top executives’ views of themselves – or rather the impression they try to convey about their activities – are not even shared by their own employees. An internal 2001 survey of Pfizer employees, which is not available to the public, showed that about 30% didn’t agree with the statement, ‘Senior management demonstrates honest, ethical behavior.
In 2012, Pfizer agreed to pay $60 million to settle a US federal investigation into bribery overseas. Pfizer wasn’t only accused of bribing doctors, but also hospital administrators and drug regulators in several countries in Europe and Asia. The investigators said Pfizer units sought to hide the bribery by listing the payments in accounting records as legitimate expenses, such as training, freight and entertainment. According to court papers, the company wired monthly payments for what it described as ‘consultancy services’ to a doctor in Croatia who helped decide what drugs the government would register for sale and reimbursement. Pfizer didn’t admit or deny the allegations, which is routine practice when drug companies settle accusations of fraud.
Hoffman-La Roche, the biggest drug pusher
The 10 largest drug companies are all signatories to the US PhRMA code, apart from Hoffman-La Roche, Switzerland, which was the largest corporate fraudster worldwide in the 1990s according to a 1999 listing of all industries, including banks and oil. High- level Roche executives led a cartel that, according to the US Justice Department’s antitrust division, was the most pervasive and harmful criminal antitrust conspiracy ever uncovered.9 Top executives at some of the world’s biggest drug companies, largely from Europe and Asia, met secretly in hotel suites and at conferences. Working together in a coalition they brazenly called ‘Vitamins Inc.’, they carved up world markets and carefully orchestrated price increases, in the process defrauding some of the world’s biggest food companies. Roche alone had revenues of $3.3 billion in the United States while the conspiracy was running, and during that time, the conspirators gradually and artfully raised the prices of raw vitamins, so as not to attract notice; they also rigged the bidding process.
The Justice Department charged Kuno Sommer, former Director of Worldwide Marketing, Hoffmann-La Roche Vitamins and Fine Chemicals Division, with participating in the vitamin cartel and for lying to Department investigators in 1997 in an attempt to cover up the conspiracy. Sommer pleaded guilty and got a 4-month prison term. After the conspiracy collapsed, those involved agreed to pay nearly $1 billion to settle federal antitrust charges, and virtually every big vitamin maker in the world was on the brink of agreeing to pay an additional $1 billion. Roche agreed to pay $500 million, equivalent to about 1 year’s revenue from its vitamin business in the United States, and two executives were sentenced to prison terms of a few months. In Europe, the European Commission fined some of the world’s biggest drug companies, including Roche, a record £523 million in 2001. It is surprising that the cartel could exist for so long, as a Roche insider blew the whistle already in 1973, which the European Commission acted on.
Between the two world wars, Roche supplied morphine to the underworld. Other drug companies in the United Kingdom, Germany, Japan, Switzerland and the United States also participated in the trade with opium, morphine and heroin. The CEO of Roche in the United States, Elmer Bobst, had great difficulty persuading his superiors in Basel that they should stop their unethical business practice. Roche continued to ship narcotics to the United States behind Bobst’s back, but he came across a cryptic telegram while visiting the headquarters, which left no doubt that it came from US criminals. It spoke about a shipment of sodium bicarbonate, which is used for baking cakes!
Roche agreed to stop the trade when Bobst reported that the US government had threatened to exclude Roche from doing business in the United States if the company didn’t stop. However, Roche took up the habit again, and again without telling Bobst. In his book, Bobst mentions that the man who was responsible for this wasn’t at heart an immoral man, but utterly amoral in business. Bobst couldn’t understand how it was possible to have two ethical standards, one for private life and one for business. He also describes how Roche avoided Swiss taxes by setting up a company in the tax refuge, Lichtenstein.
Pushing drugs that people don’t need is a highly lucrative business, particularly when the drugs affect brain functions. Roche pushed Valium (diazepam) to become the topselling drug in the world, although many indications for its use were highly doubtful and the wholesale price was 25 times the price of gold. In the early 1970s, Roche was fined by antitrust officials in Europe for engaging in anticompetitive behaviour in the sale of Valium and another best-selling tranquilliser, Librium (chlordiazepoxide).
It took 27 years after the first report about dependence had been published before the drug regulators fully acknowledged that tranquillisers are strongly addictive, just like heroin and other narcotics. I believe that the fact that some drugs affecting the brain are legal and others are illegal is irrelevant from an ethical perspective, if we try to understand what the drug industry is doing to the population. Another reason why the distinction is irrelevant is that the drug industry doesn’t really bother whether their actions are legal or not, as illustrated by the pervasive use of illegal, off-label marketing. Furthermore, what is legal isn’t static, but can change with country, fashion and prevailing beliefs. For example, narcotics haven’t always been illegal, and although it’s illegal to sell hash in most countries, it’s legal to smoke hash in the Netherlands. It is sold in so-called coffee shops, and this funny name once fooled me. Breakfasts at hotels are exceedingly expensive compared to how little most of us eat in the morning, so I went into a coffee shop one morning in Amsterdam. The owner was very amused when I asked for coffee, which he didn’t have. Shortly afterwards, three lovely girls from the Middle East entered the shop and told me that Black Lebanon was the best and that they were going to smoke just that.
As another example of legal inconsistency for substances affecting the brain, it is illegal to produce your own brandy but legal to buy it in a shop.
Whatever the legal status of brain active substances, drugs are being pushed in both cases. After having examined the drug industry in great detail, John Braithwaite published his observations in the book Corporate Crime in the Pharmaceutical Industry. In it he said:
People who foster dependence on illicit drugs such as heroin are regarded as among the most unscrupulous pariahs of modern civilisation. In contrast, pushers of licit drugs tend to be viewed as altruistically motivated purveyors of a social good.
Hall of Shame for big pharma
The BMJ comes out weekly and most issues describe one or more scandals related to the drug industry in its News section or elsewhere. The New York Times also publishes many stories about drug industry misconduct, and most of the documentation I have collected over the years comes from these two highly respected sources. In recent years, numerous articles and books have described serious cases of research misconduct and marketing fraud committed by big pharma, but although the facts are overwhelming, the standard response from the drug industry when a company has been caught is that there are a few bad apples in any enterprise.
The interesting question is whether we are seeing a lone bad apple now and then’ which might be excusable’ or whether pretty much the whole basket is rotten’ i.e. whether most companies routinely break the law.
To find out’ I did 10 Google searches in 2012 combining the names of the 10 largest drug companies with ‘fraud’. There were between 0.5 and 27 million hits for each company. I selected the most prominent case described in the 10 hits on the first Google page and supplied the information with additional sources.
The 10 cases were all recent (2007-2012) and were all related to the United States. The most common criminal offenses were illegal marketing recommending drugs for off-label uses’ misrepresentation of research results’ hiding data on harms’ and Medicaid and Medicare fraud. I describe the cases in descending order according to the size of the company.
1. Pfizer agreed to pay $2.3 billion in 2009
This was the largest healthcare fraud settlement in the history of the US Department of Justice at the time. A subsidiary of the firm pleaded guilty to misbranding drugs ‘with the intent to defraud or mislead’’ and the firm was found to have illegally promoted four drugs: Bextra (valdecoxib’ an anti-arthritis drug’ withdrawn from the market in 2005)’ Geodon (ziprasidone’ an antipsychotic drug)’ Zyvox (linezolid’ an antibiotic) and Lyrica (pregabalin’ an epilepsy drug).
An amount of $1 billion was levied to resolve the allegations that Pfizer paid bribes and offered lavish hospitality to healthcare providers to encourage them to prescribe the four drugs’ and six whistle-blowers would receive $102 million. Pfizer entered a Corporate Integrity Agreement with the US Department of Health and Human Services’ which means that good behaviour is required for the next 5 years. Pfizer had previously entered into three such agreements and when Pfizer promised the federal prosecutors not to market drugs illegally again in 2004’ Pfizer was busily doing exactly this while 27 they signed the agreement.
Pfizer’s antibiotic’ Zyvox’ cost eight times as much as vancomycin’ which even Pfizer admitted in its own fact book is a better drug’ but Pfizer lied to the doctors’ telling them Zyvox was best. Even after the FDA had told Pfizer to stop its unsubstantiated claims because they posed serious safety concerns’ as vancomycin is used for life-threatening conditions’ Pfizer continued to tell hospitals and doctors that Zyvox would save more 27 lives than vancomycin.
2. Novartis agreed to pay $423 million in 2010
The payment concerned criminal and civil liability arising from the illegal marketing of Trileptal (oxcarbazepine, an epilepsy drug approved for the treatment of partial seizures, but not for any psychiatric, pain or other uses). The company unlawfully marketed Trileptal and five other drugs, causing false claims to be submitted to government healthcare programmes. The agreement resolved allegations that the company paid kickbacks to healthcare professionals to induce them to prescribe Trileptal and five other drugs, Diovan (valsartan, for hypertension), Zelnorm (tegaserod, a drug for irritable bowel syndrome and constipation, which was removed from the market by the FDA in 2007 because of cardiovascular toxicity), Sandostatin (octreotide, a drug that mimics a natural hormone), Exforge (amlodipine + valsartan, for hypertension) and Tekturna (aliskiren, for hypertension).
The whistle-blowers, all former employees of Novartis, would receive payments of more than $25 million, and Novartis signed a Corporate Integrity Agreement.
3. Sanofi-Aventis to pay more than $95 million to settle fraud charge in 2009
According to the settlement, Aventis had overcharged US and local health agencies for medications destined for indigent patients. The Justice Department said they would ensure that programmes for the most vulnerable parts of the population did not pay any more for drugs than they should under the law. Aventis acknowledged that it misreported drug prices for patients in the Medicaid Drug Rebate programme for poor patients. The firm deliberately misquoted the prices, underpaying rebates to Medicaid and overcharging some public health agencies for the medications. The fraud occurred between 1995 and 2000 and concerned steroid-based nasal sprays containing triamcinolone.
4. GlaxoSmithKline to pay $3 billion in 2011
This is the largest healthcare fraud settlement in US history. GlaxoSmithKline pleaded guilty to having marketed a number of drugs illegally for off-label use, including Wellbutrin (bupropion, an antidepressant), Paxil (paroxetine, an antidepressant), Advair (fluticasone + salmeterol, an asthma drug), Avandia (rosiglitazone, a diabetes drug) and Lamictal (lamotrigine, an epilepsy drug).
The Justice Department charged a former vice president and top lawyer for Glaxo a year earlier with making false statements and obstructing a federal investigation into illegal marketing of Wellbutrin for weight loss. The indictment accused the vice president of lying to the FDA, denying that doctors speaking at company events had promoted Wellbutrin for uses not approved by the agency, and of withholding incriminating documents.
The company paid kickbacks to doctors, failed to include certain safety data about rosiglitazone in reports to the FDA, and its sponsored programmes suggested cardiovascular benefits from Avandia despite warnings on the FDA-approved label regarding cardiovascular risks. Avandia was withdrawn in Europe in 2010 because it increases cardiovascular deaths.
Allegations of Medicaid fraud by misreported prices were also covered by the agreement. The whistle-blowers were four employees of GlaxoSmithKline, including a former senior marketing development manager and a regional vice president. The company entered into a Corporate Integrity Agreement.
5. AstraZeneca to pay $520 million in 2010 to settle fraud case
The charges were that AstraZeneca illegally marketed one of its best-selling drugs, the antipsychotic drug Seroquel (quetiapine), to children, the elderly, veterans and inmates for uses not approved by the FDA, including aggression, Alzheimer’s, anger management, anxiety, attention-deficit hyperactivity disorder (ADHD), dementia, depression, mood disorder, post-traumatic stress disorder and sleeplessness. Further, the company targeted its illegal marketing towards doctors who do not typically treat psychotic patients and paid kickbacks to some of them. Other doctors were sent to lavish resorts to encourage them to market and prescribe the drug for unapproved uses. The whistle-blower would get more than $45 million.
The fine was small, as the drug sold for $4.9 billion in 2009. AstraZeneca denied wrongdoing although its misdeeds were obvious. The US Attorney General said about them:
‘These were not victimless crimes – illegal acts by pharmaceutical companies and false claims against Medicare and Medicaid can put the public health at risk, corrupt medical decisions by healthcare providers, and take billions of dollars directly out of taxpayers’ pockets.’
6. Roche convinces governments to stockpile Tamiflu
Roche has committed what to me looks like the biggest theft in history,but no one has yet dragged the company to court. In preparation for the mild 2009 influenza epidemic, the European and US governments spent billions of Euros and dollars on the purchase of Tamiflu (oseltamivir).
Roche has omitted publishing most of their clinical trial data and has refused to share them with independent Cochrane researchers. Based on unpublished trials, Roche has claimed that Tamiflu reduces hospital admissions by 61%, secondary complications by 67%, and lower respiratory tract infections requiring antibiotics by 55%. Curiously, the company convinced the European Medicines Agency (EMA) to approve the drug for prevention of influenza complications, and the agency’s summary of product characteristics stated that lower respiratory tract complications were reduced from 12.7% to 8.6% (P = 0.001).
In contrast, the FDA sent Roche a warning letter that the company should stop claiming that Tamiflu reduces the severity and incidence of secondary infections, and it required Roche to print a disclaimer on the labels: ‘Tamiflu has not been proven to have a positive impact on the potential consequences (such as hospitalizations, mortality, or economic impact) of seasonal, avian, or pandemic influenza.
When the FDA first reviewed a similar drug, zanamivir (Relenza) from GlaxoSmithKline, the advisory committee recommended by a vote of 13 to 4 that the drug should not be approved. In analysis after analysis, zanamivir was no better than placebo when the patients were taking other drugs such as paracetamol. Within days after this decision, Glaxo sent a fiery letter to the FDA stating that the decision was ‘completely at odds with the will of Congress that drug development and approval proceed swiftly and surely’. This threat made the FDA’s leadership overrule the committee and criticize its reviewer, biostatistician Michael Elashoff, for giving negative testimony. Elashoff was originally assigned also the oseltamivir application, but this was taken away from him and he left the agency after its demonstration of how an ineffective drug gets approved. When zanamivir was approved, the FDA also had to approve oseltamivir later the same year.
There is no convincing evidence that Tamiflu prevents influenza complications or reduces the spread of influenza to other people. However, Roche used ghostwriters, and one of the ghosts said: ‘The Tamiflu accounts had a list of key messages that you had to get in. It was run by the marketing department and you were answerable to them. At best, Tamiflu reduces the duration of influenza by 21 hours, which can likely be obtained with far cheaper drugs like aspirin and paracetamol. Furthermore, Tamiflu has important harms, but they were concealed to such an extent that the Cochrane researchers could not report on them in their Cochrane review. Even so, the Cochrane researchers found that cases of hallucination and weird accidents have been fairly commonly reported in Roche’s post-marketing surveillance of Tamiflu, in accordance with case series from Japan and experiments in rats that exhibited many of the same symptoms. A journal article signed by a group of Roche authors claimed that rats and mice given a very high dose of Tamiflu showed no ill effect, but according to documents submitted to the Japanese Ministry of Health, Labor, and Welfare by Chugai, the Japanese Roche subsidiary, the exact same dose of Tamiflu killed more than half of the animals!
If Roche’s unpublished data had really shown what the company purports they have, Roche would hardly have hesitated to share them with Cochrane researchers or to publish them. Stunningly, however, Roche has stated that the additional studies ‘provided little new information and would therefore be unlikely to be accepted for publication by most reputable journals. These claims are ridiculous. I cannot abstain at this point from quoting Drummond Rennie, editor of JAMA, who, in his announcement for the first peer review congress, stated:
‘There seems to be no study too fragmented, no hypothesis too trivial, no literature citation too biased or too egoistical, no design too warped, no methodology too bungled, no presentation of results too inaccurate, too obscure, and too contradictory, no analysis too self-serving, no argument too circular, no conclusions too trifling or too unjustified, and no grammar and syntax too offensive for a paper to end up in print.’
After much media attention, Roche promised in 2009 to make the full study reports of the unpublished trials available on its website, but this hasn’t happened.
Another curiosity is that Roche sent one of the Cochrane researchers a draft agreement, which stipulated that if signed, he could not even mention that such an agreement existed! Apparently, Roche intended not only to keep its data concealed but also the fact that it silenced people who asked for the data. The Cochrane researcher asked for clarification the next day but never received a reply.
The Council of Europe has criticised national governments, the World Health Organization (WHO) and the EU agencies for being guilty of actions that led to a waste of large sums of money. Many people have wondered why the WHO selected people to write guidance about influenza drugs who were paid by the companies marketing the drugs, and who didn’t disclose this in their guidance reports, and why there was so much secrecy around it that it wasn’t even possible for outsiders to get information on who were on the WHO committee.
WHO has been an ideal partner for Roche’s excesses and Roche has boasted that it works as ‘a responsible partner with governments to assist in their pandemic planning. Roche’s actions belie this statement, and in 2012 I suggested that the European governments should sue Roche to get the billions of Euros back they had spent on needlessly stockpiling Tamiflu, which might also have the effect that the hidden trial results came out in the open. Furthermore, I suggested we should boycott Roche’s products until they publish the missing Tamiflu data.
7. Johnson & Johnson fined more than $1.1 billion in 2012
A jury found that the company and its subsidiary Janssen had downplayed and hidden risks associated with its antipsychotic drug Risperdal (risperidone). The judge found nearly 240 000 violations under Arkansas’ Medicaid-fraud law. Jurors returned a quick verdict in favour of the state, which had argued that Janssen lied about the potentially life-threatening side effects of Risperdal which, like other antipsychotic drugs, include death, strokes, seizures, weight gain and diabetes. The FDA had ordered Janssen to issue a letter to doctors correcting an earlier letter saying the drug didn’t increase the risk of developing diabetes. Janssen continued to maintain after the verdict that it didn’t break the law. Previous verdicts against the company a few months earlier included a $327 million civil penalty in South Carolina and a $158 million settlement in Texas.
The worst of all this was that the crimes hit hard also on children. More than a quarter of Risperdal’s use was in children and adolescents, including non-approved indications, and a panel of federal drug experts concluded that the drug was used far too much. A world-renowned child psychiatrist, Joseph Biederman from Harvard, pushed the drug heavily to children and also extorted the company. Internal emails released for use in court cases revealed that Biederman was furious after Johnson & Johnson rejected a request he had made to receive a $280 000 research grant. A company spokesperson wrote: ‘I have never seen someone so angry … Since that time, our business became non-existant [sic] within his area of control.’
The fraud case could become even bigger. In April 2012, the US government stated in a motion in a potential multibillion-dollar healthcare fraud case against Johnson & Johnson that Alex Gorsky, Vice President of Marketing, who was set to become Johnson & Johnson’s next chief executive officer, was actively involved and had firsthand knowledge of the alleged fraud. The allegations were that Johnson & Johnson paid kickbacks to induce Omnicare, the nation’s largest nursing home pharmacy, to purchase and recommend Risperdal and other of the company’s drugs. The company didn’t inform Omnicare or members of Janssen’s sales staff that the FDA had warned the company that marketing Risperdal as safe and effective in the elderly would be false and misleading because the drug had not been adequately studied in that population, or that the FDA had rejected the company’s attempt to get approval to market Risperdal for treatment of psychotic and behavioural disturbances in dementia (by far the most prevalent use of Risperdal in Omnicare-served nursing facilities) because of inadequate safety data. Despite the weight of federal and state investigations of the Risperdal allegations, Johnson & Johnson’s board of directors rewarded Gorsky by selecting him to be the next CEO. It’s like in the mob: the greater the crime, the greater the advancement.
8. Merck to pay $670 million over Medicaid fraud in 2007
Merck had failed to pay the appropriate rebates to Medicaid and other government healthcare programmes, and had also paid kickbacks to doctors and hospitals to induce them to prescribe various drugs. The allegations were brought in two separate lawsuits filed by whistle-blowers, and one of them would receive $68 million. From 1997 to 2001, Merck’s sales force used approximately 15 different programmes to induce doctors to prescribe its drugs. These programmes primarily consisted of excess payments to doctors disguised as fees for ‘training’, ‘consultation’ or ‘market research’. The government alleged that these fees were illegal kickbacks intended to induce the purchase of Merck drugs. Merck agreed to a Corporate Integrity Agreement.
9. Eli Lilly to pay more than $1.4 billion for illegal marketing in 2009
Eli Lilly entered into a settlement with the Department of Justice concerning a wideranging, off-label marketing scheme for its top-selling antipsychotic drug, Zyprexa (olanzapine), with worldwide sales of nearly $40 billion between 1996 and 2009. In the settlement, Eli Lilly would pay $800 million in civil penalties and pleaded guilty to criminal charges, paying an additional $600 million fine. The allegations were raised by six whistle-blowers from Lilly who would share in approximately 18% of the federal and qualifying states’ recoveries. All whistle-blowers were fired or forced to resign by the company. According to the complaint, one sales representative had contacted the company hotline regarding unethical sales practices but received no response.
Lilly successfully marketed Zyprexa for numerous off-label uses including Alzheimer’s, depression and dementia, particularly in children and the elderly, although the harms of the drug are substantial, inducing heart failure, pneumonia, considerable weight gain and diabetes. Lilly salespeople were posed as persons in the audience who were interested in Zyprexa’s expanded use and asked ‘planted questions’ during off-label lectures and audio conferences for physicians. Another tactic was that, while knowing the substantial risk for weight gain posed by Zyprexa, the company minimised the connection between Zyprexa and weight gain in a widely disseminated videotape called The Myth of Diabetes that used ‘scientific studies of questionable integrity as well as the haphazard reporting of adverse events’. The settlement agreement included a Corporate Integrity Agreement.
10. Abbott to pay $1.5 billion for Medicaid fraud in 2012
Abbott settled allegations of Medicaid fraud for the company’s illegal marketing of the epilepsy drug Depakote (valproate); $84 million would be paid to the whistleblowers. Abbott would pay $800 million in civil damages and penalties to compensate Medicaid, Medicare and various federal healthcare programmes for harm suffered as a result of its conduct. Abbott also pleaded guilty to a violation of the Food, Drug, and Cosmetic Act and agreed to pay a criminal fine and forfeiture of $700 million.
The states alleged that Abbott promoted the sale and use of Depakote for uses that were not approved by the FDA as safe and effective; that Abbott Laboratories made false and misleading statements about the safety, efficacy, dosing and cost-effectiveness of Depakote for some unapproved uses; improperly marketed the product in nursing homes for demented patients while the company had halted a trial in such patients that showed increased adverse effects; and paid kickbacks to induce doctors and others to prescribe or promote the drug. Abbott entered into a Corporate Integrity Agreement.
It’s organised crime
In 2004-5, the Health Committee in the British House of Commons examined the drug industry in detail and found that its influence was enormous and out of control. They found an industry that buys influence over doctors, charities, patient groups, journalists and politicians, and whose regulation is sometimes weak or ambiguous. Furthermore, the Department of Health is not only responsible for the national health service but also for representing the interests of the drug industry. The committee’s report made it clear that reducing the influence of industry would be good for everybody, including the industry itself, which could concentrate on developing new drugs rather than on corrupting doctors, patient organizations, and others. The report also said that we need an industry that is led by the values of its scientists, not those of its marketing force, and the committee was particularly worried about the increasing medicalisation, i.e. the belief that every problem requires a pill.
Nevertheless, the British government did nothing in response to the Health Committee’s damning report, likely because the British drug industry is the third most profitable activity, after tourism and finance. After having been shown unequivocal and massive evidence of unhealthy industry influence on public health, government officials declared that there was no evidence of unhealthy industry influence on public health!
The Department of Health defended the industry, citing its trade surplus of more than £3 billion and argued that drug company representatives were giving doctors good information. It even defended the rising numbers of prescriptions for antidepressants although this is pretty indefensible, as I shall explain in Chapter 17. Alleged promotional excesses were dismissed with the argument that appropriate mechanisms were in place. This is what Ben Goldacre calls ‘fake fixes’. The public is repeatedly given false reassurances that the problem has been fixed.
When asked directly about whether the department understood that there was a fundamental conflict between the industry’s drive for profit and the government’s responsibility for public health, the reply was that the ‘stakeholder relationship’ between government and industry ‘brings many gains and many innovative medicines … with huge impacts on health outcomes’.
I’m speechless. With a governmental attitude of total denial it’s no great wonder that crime flourishes in the drug industry and spreads like weeds.
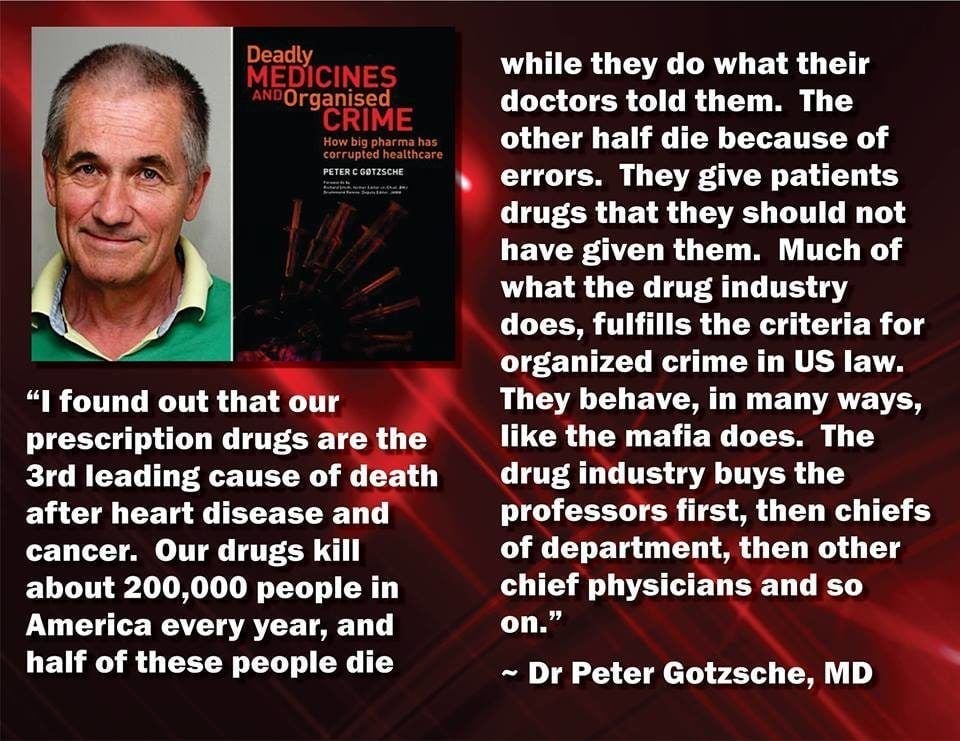
The centrepiece of the US Organized Crime Control Act from 1970 is the Racketeer Influenced and Corrupt Organizations Act (RICO).91 Racketeering is the act of engaging in a certain type of offense more than once. The list of offenses that constitute racketeering include extortion, fraud, federal drug offenses, bribery, embezzlement, obstruction of justice, obstruction of law enforcement, tampering with witnesses, and political corruption. Big pharma does so much of this all the time that there can be no doubt that its business model fulfills the criteria for organised crime.
Remèdes mortels et crimes organisés
est un ouvrage essentiel
qu’il est impardonnable de ne pas avoir lu
Et les conséquences de ce péché par omission
sont morelles et pourtant multirécidivistes